Joint Work (Including Integrated Neighbourhood Working)
Amendment
In August 2025, contact details were updated in Section 5, Integrated Neighbourhood Working.
This guidance has been written to support any Local Authority practitioner who will be working jointly with:
- another Local Authority practitioner; or
- a practitioner from another organisation (for example, health or education).
It sets out:
- the forms that joint work can take;
- some of the benefits of joint work;
- some general principles for good joint work.
Broadly speaking, joint work can be defined as:
- a process involving more than one practitioner; where
- a co-operative approach is taken; to
- benefit a person with care and support needs, or a carer with support needs.
Joint work can take many forms, many of which can apply at the same time:
|
Nature |
Description |
Example |
|---|---|---|
|
Low level |
Basic functions and information sharing |
Information sharing after a verbal request Co-operating with small tasks and functions to carry out a process |
|
High level |
Complex work or functions |
Shared assessment Multi-agency safeguarding Determining eligibility for NHS Continuing Healthcare |
|
Single agency |
Local Authority joint work |
A social worker and an Occupational Therapist A safeguarding officer and a community care officer |
|
Multi-agency |
Joint work across more than one agency |
Integrated health and social care teams An Occupational Therapist and a Physiotherapist A social worker and a teacher |
|
Informal |
Joint work that does not require a formal request |
Contacting a nurse to request information about health needs Contacting a teacher to confirm a young person's needs at college |
|
Formal |
Subject to a formal request |
Referral for an assessment A request to be part of a safeguarding MDT |
|
Direct |
Involving the person or carer |
Determining eligibility for NHS Continuing Healthcare A joint funding assessment A joint social work/OT assessment |
|
Indirect |
No direct involvement of the person or carer |
Liaising with the Direct Payment team to arrange a Direct Payment Liaising with the Brokerage team to identify available care home placements |
Good joint work has many benefits, some of which are set out in the table below:
|
Benefit to the Person or Carer |
Benefit to the Organisation |
|---|---|
|
A holistic approach to meeting their needs, rather than a staggered one. |
Shared resources (time and services). |
|
Reassurance that complex or multiple needs are being met in the right way. |
Reduced administrative burden if tasks can be shared. |
|
Only having to provide information once. |
A wider range of available options to meet needs. |
|
Having access to all relevant information and expert advice at the same time. |
More effective processes. |
|
More timely decision making. |
A greater understanding of the roles and responsibilities of others. |
|
More sustainable outcomes. |
More robust decision making through the appropriate challenge of others. |
Under section 6 of the Care Act:
- the Local Authority must co-operate generally with relevant partners; and
- relevant partners must co-operate with the Local Authority; when
- that co-operation is required to ensure that care and support functions are carried out; or
- when carrying out more localised functions relating to other statutory duties and responsibilities.
If a formal request is made in writing for joint work (for example, through a referral), the person receiving that request must co-operate with it unless:
- doing so will prevent them from carrying out their own duties under the Care Act or any other legislation; or
- doing so will prevent them from exercising any of their other functions; in which case
- they must provide a written explanation of their reasons for declining to the person making the request.
Integrated neighbourhood working empowers local people to take an active role in their health and wellbeing with greater choice and control.
It will keep people independent for as long as possible and help to avoid unnecessary hospital admissions. Essential services in the team include:
- General Practice (GPs);
- Nursing services;
- Therapy services;
- Mental Health services;
- Social Care services;
- Reablement.
These professionals are linked into the local community and can ensure that residents get a genuinely joined up approach from wider support services. By bringing together health, social care, and community in a person-centred approach, we can empower individuals to live more independently and provide support to manage their care more effectively.
Neighbourhood working means:
- strengthening and re-designing community services to meet local needs, to include better coordination and communication locally;
- proactively supporting people at risk of deteriorating ill health;
- focusing on what individuals can do and supporting them to achieve their goals;
- supporting staff to work in partnership with shared information to provide joined up care;
- supporting faster access to the right help and support, including linking with voluntary groups and charities available in the local area;
- proactively supporting people, when they need it, providing the right support at the right time.
Note: Neighbourhood working should be used where people with complex or long term conditions would benefit from a joint assessment and planning.
Neighbourhood Working in Lincolnshire brings together people working in the health, care, housing, and community voluntary sectors, with a focus on improving the health and wellbeing of local populations. Each neighbourhood will have different challenges relating to its unique geographical and demographic conditions, and teams work together to identify opportunities and solutions to support some of our most vulnerable people in our local populations. There are seven principles of neighbourhood working:
- Home First – working together to manage risk and enable people to receive the right care closest to home;
- Population Health Management – understanding local needs and priorities across the local population;
- Accessible Information – ensuring people are aware of all options and opportunities to stay well;
- Care Navigation – getting the right intervention at the right time, utilising all neighbourhood resources;
- Social Prescribing – connecting people to their communities and addressing isolation;
- Personalised Assessment, Care and Support Planning – proactive and anticipatory care which helps people stay well and respond appropriately at times of deterioration or crisis;
- Personalised Outcomes, Delivery and Review – focusing on what matters to the person and having a positive impact.
Neighbourhood Working:
- helps break down organisational silos and promote collaborative approaches, supporting professionals to work more creatively and flexibly to support people;
- promotes holistic approaches that empower people to have control over their health and wellbeing – balancing correct clinical intervention with the support of non-clinical and community assets;
- helps model and shape values across the health and care system which put people at the centre of their care and support;
- enables joint contributions to people’s care and support planning, promoting independence and sharing risk;
- helps remove duplication and inefficiency by ensuring the most appropriate interventions are being offered at the most appropriate time;
- identifies people with most complex needs who are, or at risk of becoming, high intensity users of services to develop plans to manage complex needs.
The Neighbourhood teams in Lincolnshire are divided into 3 clusters; West, East and South.
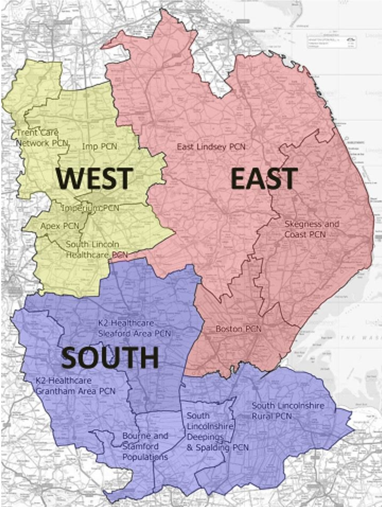
The contact details for each cluster are:
West
Email: Lhnt.nhwest@nhs.net
Covering: Apex, IMP, Heart of Lincoln, South Lincoln Healthcare, and Trent Care Network.
East
Email: licb.east-neighbourhoods@nhs.net
Covering: Boston, East Lindsey, First Coastal, Meridian Medical, and SOLAS.
South
Area: South
PCN: South Lincs Rural
Email: slccg.neighbourhoodteam@nhs.net
Member Practices:
Gosberton Medical Centre
Sutterton Surgery
Galletly Practice
Abbeyview Surgery
Holbeach Medical Centre
Littlebury Medical Centre
The Suttons Medical Group
Deepings Practice
Moulton Medical Centre
Area: South West Lincolnshire
PCN: K2Healthcare Sleaford & Grantham and Rural PCNs
Email: swlccg.inw@nhs.net
Member Practices:
Colsterworth Medical Practice
Long Bennington Medical Centre
Market Cross Surgery
St John’s Medical Centre
St Peter’s Hill Surgery
Swingbridge Surgery
Glenside Country Practice
Vine Street Surgery
Ruskington Medical Practice
Caythorpe & Ancaster Practice
Sleaford Medical Group
The New Springwells Practice
Millview Medical Centre
Billinghay Medical Practice
Harrowby Lane Surgery
The Welby Practice
Area: Spalding
PCN: Spalding PCN
Email: licb.snn@nhs.net
Member Practices:
Beechfield Medical Centre
Munro Medical Centre
Area: Stamford
PCN: Four Counties PCN
Email: licb.fourcountiespcn@nhs.net
Member Practices:
St Mary’s Medical Centre, Stamford
Sheepmarket Surgery, Stamford
Hereward Practice, Bourne
Lakeside
The following table sets out:
- some of the general principles for good joint work; and
- some examples for applying them.
|
Principle |
How to apply |
|---|---|
|
Professional courtesy |
Make contact when you say you will Provide information as agreed Return calls and respond to e-mails Value the contribution of others Use appropriate language and have professional respect for all / for each other Inform of any delays or issues when they arise Raise any concerns about the actions (or inactions) of another practitioner appropriately |
|
Understand roles |
Make sure the other practitioner understands your role, and any limitations Make sure you understand their role-ask questions if you need to Be clear about the tasks that you need to carry out Make sure you understand the tasks that they need to carry out-ask questions if you need to |
|
Set expectations |
Be clear about all expectations for the joint work across all organisations involved Identify any potential issues and take steps to prevent them arising Expectations could include:
|
|
Agree tasks and functions |
Identify all of the different tasks and functions and agree who will carry them out. Think about:
|
Joint work can only take place if the person consents unless:
- the person lacks capacity to consent; and
- a Deputy or Lasting Power of Attorney provides consent in their Best Interests; or
- where there is no Deputy or Lasting Power of Attorney, the Local Authority makes a Best Interest decision to this effect.
The only occasion when direct joint work can take place without the consent of the person is when it is taking place as part of a safeguarding enquiry.
In the case of carers, direct joint work can only take place with their consent.
When joint work between practitioners in the same agency is required to effectively arrange services, the consent of the person or carer can be assumed if:
- the person has consented to the service being arranged; and
- the joint work is for the sole purpose of arranging the service.
(e.g. arranging a Direct Payment with the Direct Payment Team).
If there are likely to be delays in allocation or commencement of joint work, the person who requested the joint work will need to:
- consider whether to proceed with their intervention; or
- await allocation (or availability) of the other practitioner.
It is the responsibility of the person requesting joint work to make this decision (in agreement with the person and any carer) and to take steps to ensure that any urgent needs for care and support are met.
All recording of joint work should be made in line with local joint working protocols.
If in any doubt about the need for you to make a record, you should always make a record.
Joint work can involve working closely with other practitioners and professionals, during which time you will observe aspects of their practice. If you are concerned that any aspect of their practice:
- compromises the safety or wellbeing of a person with care and support needs; or
- compromises the safety or wellbeing of a carer with support needs; or
- compromises the safety of a child;
- you must use the whistleblowing procedure to raise your concern;
- regardless of the organisation that the practitioner or professional works for.
See the Whistleblowing Procedure.
Last Updated: August 12, 2025
v67